
“Prepare the machine, protective gear, and get started,” Dr. Pham Van Phuc, Deputy Director of the Intensive Care Center, Central Hospital for Tropical Diseases, had just finished speaking when the entire team was already moving around the intensive care room. An emergency bronchoscopy was performed immediately.
The 40-year-old woman lay motionless, her body emaciated after months in the hospital. She had undergone aortic arch replacement surgery at a central hospital, then was transferred to a provincial hospital for monitoring.

However, the long hospital stay caused bacteria to "take over" her body like an invisible enemy.
At the provincial hospital, the patient was diagnosed with multidrug - resistant Pseudomonas aeruginosa infection.
This is a type of bacteria that is resistant to most common antibiotics. After a month of treatment, the patient's condition did not improve. The high fever persisted, her breathing became increasingly rapid, and she eventually fell into septic shock and had to be transferred to the Central Hospital for Tropical Diseases.
The endoscope slid deep into the airway, revealing streaks of red, swollen mucosa on the screen.
Dr. Phuc explained: “The important goal is to get the deepest sample, at the exact location of the infection to determine the cause. Only when we find the culprit, can we choose the right treatment for the cause.”

For patients dependent on ventilators, the risk of infection is always lurking. Pseudomonas aeruginosa, methicillin-resistant Staphylococcus aureus (MRSA), Klebsiella pneumoniae , Acinetobacter baumannnii are familiar but also haunting names for resuscitation doctors.
They not only hide in the airways, but can also invade the blood, brain and meninges, urinary and digestive systems, causing patients to quickly suffer multiple organ failure.
In such cases, microbiological and antibiotic susceptibility testing is the “light of the road”. They help determine which bacteria are present, which antibiotics they are resistant or sensitive to, and even whether the bacteria carry resistance genes.
This is an important basis for doctors to come up with an accurate treatment plan, instead of groping in the dark.
This 40-year-old patient is just one of dozens of infectious cases that are sampled every day. There are elderly women over 80 years old who have repeated hospital-acquired pneumonia, and there are healthy young men who suddenly collapse from encephalitis with infection.
What they all have in common is an answer: What kind of bacteria is the real culprit? And what drugs are still effective to save them?

The destination for samples that need to be solved, the Department of Microbiology and Molecular Biology, with its modern equipment system and the hurried pace of staff, can receive samples 24/7. This place is considered as the "Tracing Center" for pathogens.

Each specimen from the clinical departments is treated as a valuable “clue”. Upon receipt, the technician scans the code to display patient information, ensuring that the sample is not mistaken. The data is immediately updated into the system, connected to the entire hospital.
In the sample transport box, the patient's blood tube and sputum were just brought in. Nurse Le Thi Thuy Dung quickly handed them over to her colleagues in the Microbiology laboratory. The blood sample was cultured to increase the growth of bacteria in a special medium bottle, the sputum had to go through a treatment step to remove impurities before culturing.
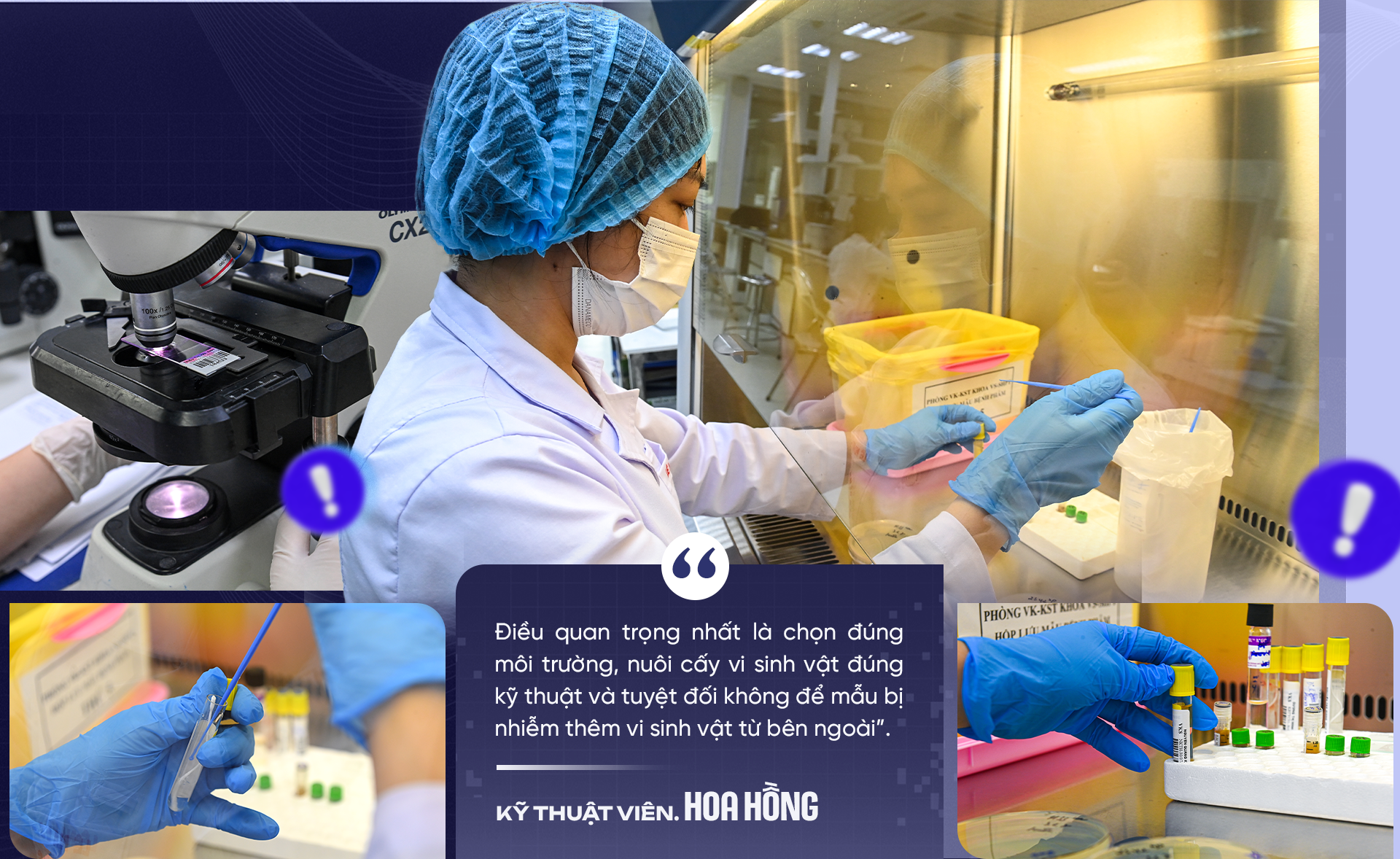
“The most important thing is to choose the right environment, cultivate microorganisms with the right technique and absolutely not let the sample be contaminated with microorganisms from outside,” shared Le Thi Hoa Hong, a technician with many years of experience.
Technical operations are performed in biosafety equipment, each step of inoculating specimens (which may contain pathogens) into her specific nutrient medium agar plate is performed precisely. The inoculating rod is a disposable type, sterilized with gamma rays before touching the sample.
The inoculated plate is then placed in an incubator where the ideal temperature and humidity are maintained for their growth. This process lasts from 24 to 72 hours or longer depending on the growth of each microorganism.

After a period of incubation, tiny colonies begin to appear on the agar plate - traces of bacteria.
Technician Hong and his colleagues selected colonies suspected of causing the disease, standardized the turbidity, then entered them into identification cards and antibiotic resistance tests, and transferred them to the Vitek 2 compact automatic system.
The machine will identify bacteria based on biochemical reactions and simultaneously perform antibiotic susceptibility testing, which means "testing" bacteria with a series of antibiotics to determine which drugs are still sensitive and which are resistant.
“The results will show the minimum inhibitory concentration (MIC), thereby classifying bacteria as sensitive, intermediate or resistant to each type of antibiotic,” shared Dr. Van Dinh Trang, Head of the Department of Microbiology and Molecular Biology.
However, the machine does not always have enough antibiotics available to test.
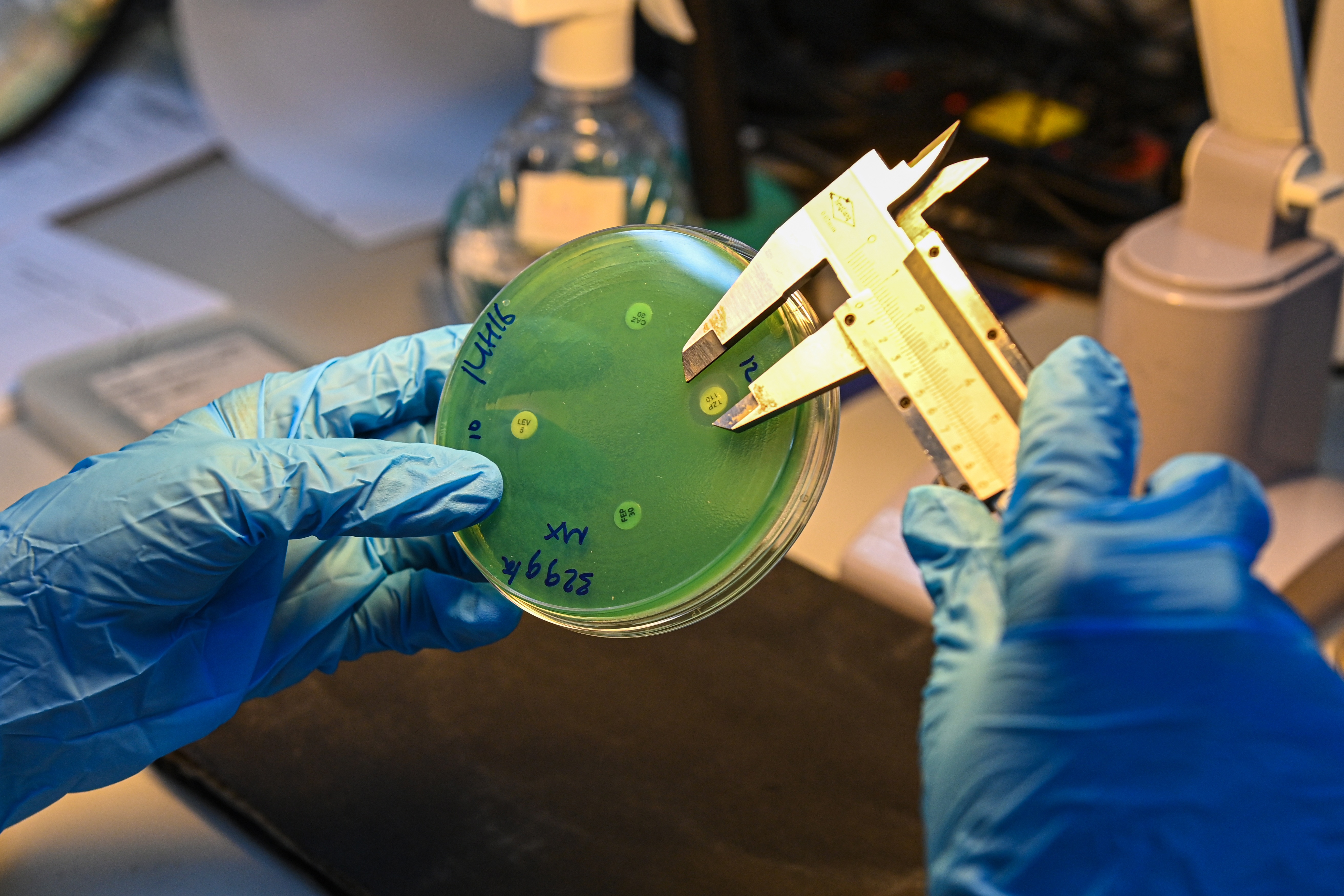
According to Dr. Trang, with rare, strange bacterial strains or those showing unusual resistance, technicians must return to the traditional method: using paper rings pre-soaked with antibiotics at a certain concentration to conduct the method of diffusing antibiotics into agar plates.
On the petri dish, each piece of antibiotic-soaked paper is placed on the surface of the agar inoculated with bacteria, then the diameter of the inhibition zone is measured to determine the level of antibiotic sensitivity or resistance of that bacteria.
Another helper is the MALDI-TOF machine. The technology of identifying bacteria by protein spectrum can give results in just a few minutes/sample.
“Each identification tray can hold up to 96 different samples. Thanks to that, we can process dozens of specimens in one session, significantly shortening the waiting time for patients,” explained Dr. Pham Thi Dung, Department of Microbiology and Molecular Biology.
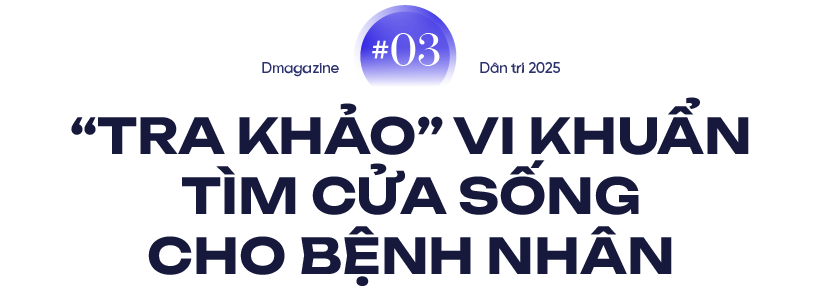
Once the specimen has been cultured and identified, the work of the Microbiology staff does not stop. This is when they enter the important stage: reading and analyzing the antibiotic susceptibility test.
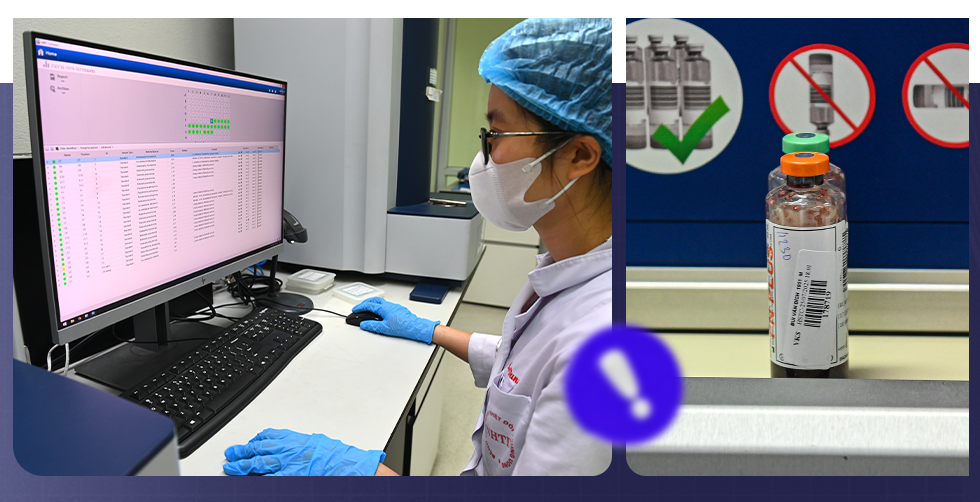
On the desk, Dr. Pham Thi Dung looked intently at the screen displaying the results from the Vitek system. The data table was dense with symbols, the MIC (minimum inhibitory concentration) index appeared next to the name of each antibiotic.
For each bacterial strain, the system automatically suggests a level of sensitivity, intermediate or resistance. But before being passed on to the clinician, all must be confirmed by the Microbiology department staff for testing, comparison and approval.
“The machine only gives out raw data. Our job is to analyze whether the results are reasonable and compatible with the characteristics of this type of bacteria. If we find anything unusual, we have to do more testing using other methods,” Dr. Dung shared.

Sometimes a strain of bacteria turns out to be resistant to almost every drug in the antibiotic arsenal. In that case, technicians are forced to perform additional genotyping tests to find out if the bacteria carry a particular resistance gene.
Only when knowing clearly the "weapons" that bacteria possess, can doctors choose the medicine that can kill or inhibit them.
During the peak of the Covid-19 epidemic, the workload at this “tracing center” increased many times.
“There were days when we almost ate and slept right in the lab. When the phone rang to announce a new case, everyone immediately got into position and worked all night to get the results as soon as possible,” Dr. Dung recalled.
When the final results are available, the female doctor will prepare a detailed report, clearly stating the name of the bacteria and the sensitivity level to each antibiotic. “I always analyze according to antibiotic stratification, giving priority drug groups and preventive drug groups, so that clinicians have a basis to choose the most optimal option,” Dr. Dung explained.
A test result is just a few lines of text, but behind it are many hours of meticulous, professional work. It can decide whether a patient is saved or not.
“We understand that each result we provide is not only scientific data but also the patient's hope of life,” Dr. Dung said, his eyes still glued to the antibiotic diffusion circles on the culture dish.

A week after the results of the antibiotic susceptibility test were returned from the Microbiology and Molecular Biology Department, the 40-year-old woman was able to sit up on her own for the first time. She smiled and thanked the doctors: “I thought I had no chance.”
The recovery began with the results of the antibiotic susceptibility test sent to the intensive care unit. From the detailed data table on the type of bacteria and the sensitivity and resistance to each drug, the treating physician was able to develop a targeted treatment regimen.
The drug-resistant Pseudomonas aeruginosa, which had previously caused the patient to go into shock and experience persistent high fever, was finally brought under control. Respiratory parameters stabilized, and the fever gradually receded.
The day she was discharged, the whole family hugged each other at the hospital gate. That joyful reunion had the silent but extremely important presence of the “bacteria hunters”. They were not present at the hospital bed, did not hold a stethoscope or a syringe, but each result they returned contributed to opening up a chance for life for the patient.
Source: https://dantri.com.vn/suc-khoe/ven-man-nghe-la-cua-nhung-tho-san-vi-khuan-20251014160424246.htm



![[Photo] Immerse yourself in the colorful musical world of “Secret Garden Live in Vietnam”](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/10/18/1760805978427_ndo_br_thiet-ke-chua-co-ten-41-png.webp)
![[Photo] Closing ceremony of the 18th Congress of Hanoi Party Committee](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/10/17/1760704850107_ndo_br_1-jpg.webp)
![[Photo] General Secretary To Lam attends the 95th Anniversary of the Party Central Office's Traditional Day](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/10/18/1760784671836_a1-bnd-4476-1940-jpg.webp)

![[Photo] Collecting waste, sowing green seeds](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/10/18/1760786475497_ndo_br_1-jpg.webp)



























































































Comment (0)