Ho Chi Minh City Ms. Ngoc, 28 years old, often has sudden seizures, epilepsy treatment for more than 8 years was ineffective, the doctor examined and discovered a congenital brain defect.
3 Tesla MRI results showed that the patient's brain had a large fissure (2-5 cm wide depending on location), extending from the cerebral cortex to the ventricle, located on the right cerebral hemisphere.
On November 10, Master, Doctor Chu Tan Si, Head of the Department of Neurosurgery, Tam Anh General Hospital, Ho Chi Minh City, said that the patient had a brain fracture since childhood but did not know it. Now the fracture has widened, causing severe epilepsy and convulsions. For the past 8 years, the patient has been treated for seizures and epilepsy with the highest dose of medication but with no results.
Brain fissure is a congenital malformation with an incidence of about 1/100,000 people, caused by a disorder of neuronal migration, according to Dr. Tan Si. The cleft changes the circulation of cerebrospinal fluid. In normal people, cerebrospinal fluid flows from the lateral ventricle to the third and fourth ventricles, then to the cerebrospinal fluid space around the brain. When a large brain fissure appears, cerebrospinal fluid flows directly from the lateral ventricle through the cleft and to the cerebrospinal fluid space, skipping some necessary stages.
According to Dr. Si, people with microcephaly can adapt and live normally. In Ms. Ngoc's case, the crack widened over time, causing cerebrospinal fluid to flow in, increasing intracranial pressure, compressing the surface of the cerebral cortex, causing epileptic seizures. The optimal solution is decompression surgery, followed by continued monitoring and treatment of epilepsy.
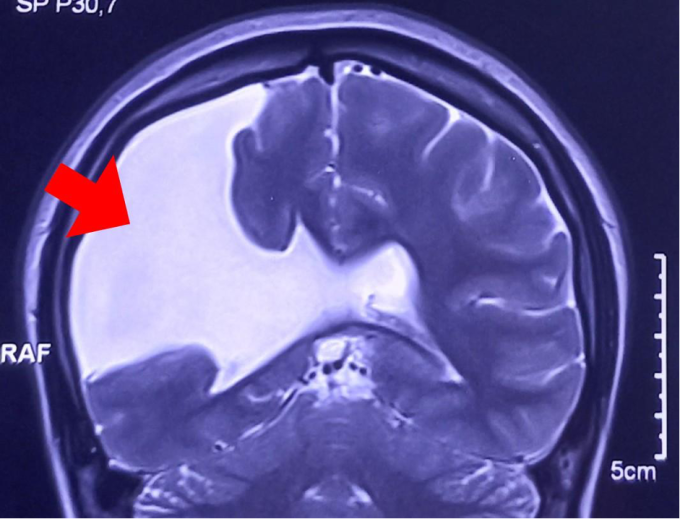
Brain MRI scan shows a large brain fissure filled with cerebrospinal fluid (white part). Photo: Provided by the hospital
The surgeon performs endoscopic decompression of the intracranial pressure, placing a specialized plastic tube into the brain fissure and passing it down to the peritoneal cavity under the abdomen. On the tube there is an automatic valve that helps maintain a moderate amount of cerebrospinal fluid, stabilizing intracranial pressure. When the cerebrospinal fluid in the brain fissure increases, increasing intracranial pressure, the tube automatically unlocks to allow the cerebrospinal fluid to flow down to the peritoneal cavity. When the cerebrospinal fluid decreases, the valve automatically locks, preventing the cerebrospinal fluid from decreasing too much.
After three days of surgery, the patient's health is stable, recovering well, and is expected to be discharged after 5 days.

Surgeons perform cerebral decompression surgery on a patient. Photo: Provided by the hospital
Dr. Tan Si said that patients need to take anti-epileptic drugs at appropriate doses. Doctors monitor changes in cerebrospinal fluid and intracranial pressure, epileptic seizures for 2-6 months and adjust anti-epileptic drug prescriptions accordingly. The goal is to switch from polytherapy to monotherapy, from taking anti-epileptic drugs at the highest dose to the lowest dose, helping patients gradually improve their health and quality of life.
Truong Giang
* The patient's name has been changed
| Readers ask neurological questions here for doctors to answer |
Source link





































![[Photo] The 1st Congress of Phu Tho Provincial Party Committee, term 2025-2030](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/9/30/1507da06216649bba8a1ce6251816820)
![[Photo] President Luong Cuong receives President of the Cuban National Assembly Esteban Lazo Hernandez](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/9/30/4d38932911c24f6ea1936252bd5427fa)
![[Photo] Solemn opening of the 12th Military Party Congress for the 2025-2030 term](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/9/30/2cd383b3130d41a1a4b5ace0d5eb989d)
![[Photo] Panorama of the cable-stayed bridge, the final bottleneck of the Ben Luc-Long Thanh expressway](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/9/30/391fdf21025541d6b2f092e49a17243f)


































































Comment (0)