Doctor used needle as thread to save "angel" with pleural effusion in mother's womb ( Video : Minh Nhat - Linh Chi).
The 23-year-old woman was pregnant for the first time at the 30th week of pregnancy. Ultrasound results at the Fetal Intervention Center, Hanoi Obstetrics and Gynecology Hospital showed that the left pleural cavity of the fetus contained a large amount of fluid, the lung parenchyma was collapsed, and the heart and mediastinum were completely displaced to the right.

After consultation and ruling out genetic abnormalities, the team agreed to place a pleural shunt to create a pathway between the pleural cavity and the amniotic cavity, helping to drain fluid, relieve lung compression, and improve fetal breathing.

At exactly 9am, the medical team at Hanoi Obstetrics Hospital was ready to enter the battle to "rescue" the fetus with a dangerous disease.
According to Dr. Phan Thi Huyen Thuong, Deputy Director of the Fetal Intervention Center, this is a condition of pleural effusion with mediastinal compression. If not treated promptly, the fluid will increase rapidly, causing fetal edema, heart failure and can cause serious disadvantages for the child after birth.


Before the procedure, the patient is given local anesthesia, the entire abdominal area is sterilized, and covered with a sterile towel.
“Cases of pleural effusion that can be treated are usually performed when the fetus is over 16 weeks old, but are most concentrated in the period of 20-34 weeks, when the lung structure and pleural cavity of the fetus have clearly formed,” said Dr. Thuong.

At 10:30, the team officially began the intervention. The ultrasound results brought good news: the fetal heart rate was good and stable.
Dr. Thuong said that one of the biggest challenges when intervening in the fetus is the position of the fetus.
“In many cases, the baby is in an unfavorable position, making it very difficult to access the area that needs intervention,” Dr. Thuong informed.
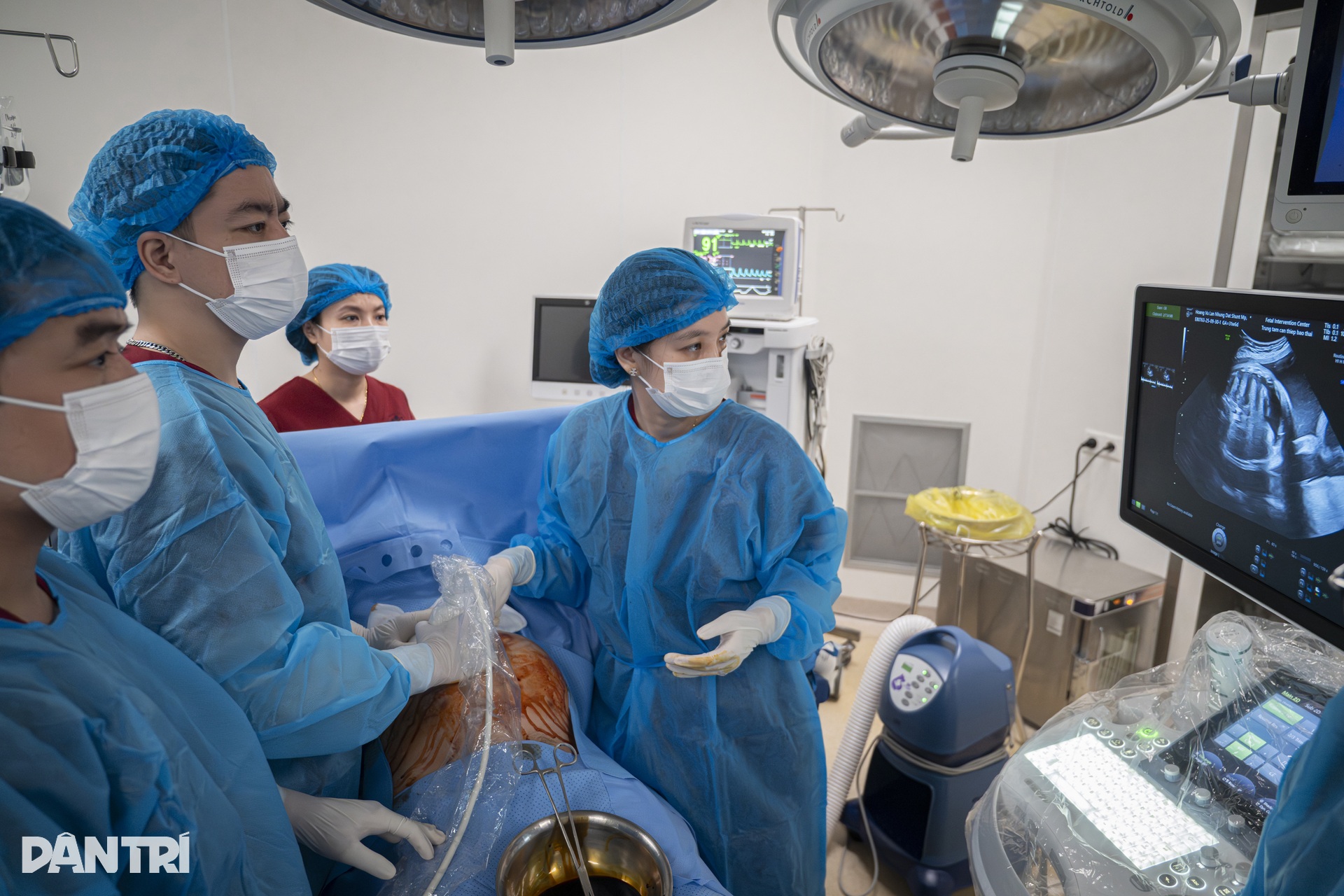
First, the team must adjust the fetal position to facilitate access to the pleural effusion area.
“There are cases where the fetus has fluid on both sides, so we have to insert two drainage tubes. After one side is done, we have to turn the baby upside down to reach the other side,” Dr. Thuong shared.

The team must accurately determine the fetal position through ultrasound. The fetal intervention team plans the path of the drainage needle, accurately calculating the route from the mother's abdominal skin, through the uterine muscles, into the amniotic sac and reaching the fetal chest wall.
According to Dr. Thuong, this is an extremely meticulous technique, because it is not possible to puncture directly into the baby's chest wall, but must go through many layers of tissue with very narrow gaps.
Typically, the team chooses the intervention site in the fetal side armpit or posterior back. These locations help reduce the risk of the drainage tube slipping out or prevent the fetus from accidentally touching, pulling, or pushing the tube out of position.

At 10:50, the team quickly determined the baby's position was favorable and anesthetized the fetus to fix the position, avoiding the baby from rotating or moving, which could make it difficult to insert the drainage tube.


After accurately locating the access point on ultrasound, the doctor uses a tiny blade to make a 2mm incision on the mother's abdominal skin, then inserts a 17mm long needle straight into the amniotic sac.

The goal of the procedure is to create a pathway between the pleural cavity and the amniotic sac, allowing the fluid that is compressing the baby's lungs to drain.
The two ends of the drainage tube must be positioned precisely: one end lies within the pleural cavity, the other end opens into the amniotic sac.


“It sounds simple, but in reality every millimeter of movement is a life-or-death calculation,” Dr. Thuong said, his eyes never leaving the ultrasound screen.
On the ultrasound screen, the needle glows like a thin streak, slowly passing through the skin of the abdomen, through the muscle layer, and then through the wall of the mother's uterus.

The needle gently glides through the tiny chest wall, reaching the pleural cavity - the fluid-filled cavity that is compressing the fetus's small lungs.
The entire operating room held its breath.
Every operation is controlled by Dr. Thuong through ultrasound images, every heartbeat, every small change of the baby is calculated to avoid errors of even a millimeter.

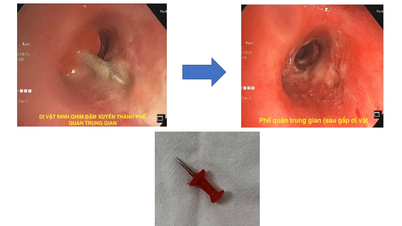
Once the shunt was placed, Dr. Thuong slowly pulled out the needle, leaving only a small, thread-like tube in the amniotic sac.
One end of the tube fits neatly in the pleural cavity, where the small heart is compressed, the other end opens into the amniotic sac, creating an "escape" so that the pressure in the baby's chest is released, allowing the baby's heart to beat normally again.
About 5 minutes later, on the ultrasound screen, the miracle began to happen: the fluid in the pleural cavity gradually decreased, the baby's lungs became brighter, and the image of the small lungs was expanding little by little.

"The baby's lungs are starting to expand," Dr. Thuong pointed to the bright areas gradually expanding in the baby's chest.
The team continued to check the entire line, making sure the drainage tube had not slipped out. Only when everything was stable and the ultrasound showed that the lungs continued to expand evenly, did Dr. Thuong gently remove the instrument.
“After 24 to 48 hours, the fluid will be drained completely. At that time, the baby's lungs will fully expand and the airways will be clear. Everything will return to normal,” Dr. Thuong said, her voice softening as if she had just walked out of a silent battle in the womb with the “angel”.
If polyhydramnios is present, the doctor may remove some of the amniotic fluid to reduce pressure in the amniotic cavity, helping to drain fluid from the pleural cavity more easily, so that the baby can breathe more easily in his or her "home".
After the intervention, the fetus will be continuously monitored by ultrasound to assess the progress of fluid drainage and lung condition.

Doctors observe whether the fluid in the pleural cavity continues to drain evenly, whether it re-accumulates on the opposite side, or whether the drainage tube falls out of place as the fetus moves through the amniotic sac.
In addition, doctors evaluate the degree of lung expansion and lung parenchyma structure, to see if there are any underlying abnormalities causing pleural effusion. In the pre-intervention stage, due to lung collapse, these details are often not clearly observed.
On the mother's side, because she has undergone an invasive procedure, she is closely monitored for the risk of infection, amniotic fluid leakage, or uterine contractions.
Fetal thoracentesis is a minimally invasive intervention that relieves lung compression, prevents fetal edema, and improves respiratory function, resulting in a high success rate and good prognosis for fetuses with pleural effusion.
Source: https://dantri.com.vn/suc-khoe/bac-si-dung-kim-nhu-soi-chi-cuu-thien-than-tran-dich-phoi-trong-bung-me-20251016190905591.htm


![[Photo] Prime Minister Pham Minh Chinh chairs meeting on nuclear power plant construction](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/10/22/1761137852450_dsc-9299-jpg.webp)









































































































Comment (0)