On the construction and implementation of the Health Insurance Appraisal Information System
In 2017, the Health Insurance Appraisal Information System with initial design according to business requirements included 2 components: Reception Portal and Health Insurance Appraisal software.
- The receiving portal is managed by the IT Center, connecting data with 12,380 medical facilities from commune to central level;
- The Health Insurance Appraisal software provides functions for 11 operations of the appraisal process.
Health Insurance Assessment Information Portal.
From 2018 to present, the System continues to be developed, completed and built with additional functions and features to help improve the efficiency and effectiveness of health insurance appraisal work, strictly and effectively control the health insurance fund, promptly detect and prevent abuse and profiteering of the health insurance fund.
The Data Receiving Portal has adjusted the functions of issuing temporary health insurance card codes, adding the function of issuing social insurance leave certificates, the function of checking the logic of payment request data, the function for medical examination and treatment facilities to authenticate electronic data, the function of looking up health insurance card information by social insurance code, on the VssID application, the VNEID/CCCD application with chip, the function of requesting temporary codes for medical supplies.
The Health Insurance Appraisal Software has been adjusted and supplemented with functions and forms for settlement of health insurance expenditures in 2020 and 2021, updated with new rules for appraising payment request data, rules for checking lists, checking health insurance contracts, notifying appraisal results, and integrating digital signatures on business reports.
Connect with TST software to update and track initial registration subjects at all levels, connect data with centralized accounting software to manage advances and payments for health insurance at each health facility, connect reports with Settlement Appraisal software to conduct settlement appraisal from 2020 at the Central level, function of approving temporary codes for medical supplies for provincial and central levels (Current Appraisal software has 230 functions with more than 300 appraisal rules).
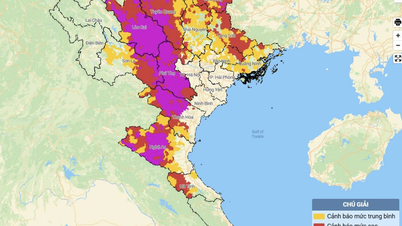
The Health Insurance Monitoring Software has been supplemented with additional functions, maps, and charts; integrated with map and chart display, especially the calculation tables of the national, provincial, and medical examination and treatment facility quota funds, helping provincial Social Insurance agencies clearly understand the fund calculation method, the national and regional general index tables, convenient for monitoring and comparison in each locality.
The Drug Management Software is deployed with the functions of analyzing the use of drug groups, active ingredients and each product; analyzing ABC/VEN (correlation between annual drug consumption and cost to identify drugs that account for a large proportion of the Health Insurance Fund) and DDD (correlation between annual drug consumption and cost to identify drugs that account for a large proportion of the Health Insurance Fund); monitoring the use of drugs in centralized bidding at the national level and local bidding, supporting the development of bidding plans, monitoring the management of drug supply, use and payment at the central level.
Results achieved:
After operation, the System has connected data between the Social Insurance agency and nearly 13,000 health insurance facilities nationwide, the quality of data connection has been significantly improved and enhanced.
Through the development of appraisal topics and the implementation of appraisals according to the topics, the Social Insurance of the provinces will recover to the Health Insurance Fund cases of illegal payments.
The information is updated and transparently disclosed regularly on the System, helping local Social Insurance agencies easily identify and quickly detect changes and developments between periods and months to promptly coordinate with medical facilities in controlling the effective use of the Health Insurance Fund. Many medical facilities have made positive changes in treatment indications, contributing to reducing unnecessary expenses.
In policy development, the Health Insurance Database has become the main source of information to assess impacts and adjust policies, develop new health insurance payment methods according to quotas and diagnostic groups, evaluate and select new drugs and technologies into the health insurance benefit package.
Impact of digital transformation in health insurance appraisal
For health insurance patients:
Significantly reducing waiting time for medical examination and treatment, information about health insurance cards is looked up online and updated directly into the medical examination and treatment management software of the medical facility. Cases of card renewal and conditions for exemption from co-payment are updated immediately to help patients be fully assured of medical examination and treatment benefits while being treated at the hospital.
Patients can look up information about treatment costs, services used, and transparency in health insurance benefits, while enhancing the role of health insurance participants in controlling the use of health insurance funds.
For medical facilities:
Update information on health insurance cards accurately and promptly, limiting errors when creating medical records and requesting health insurance payments.
Track medical examination and treatment history, convenient for medical examination and diagnosis.
Sharing clinical and treatment results between medical facilities helps reduce unnecessary repeat prescriptions.
Prevent the abuse of health insurance cards for medical examination and treatment at many medical facilities.
Actively monitor the use of medical examination and treatment funds at the unit and proactively adjust unreasonable expenditures.
For social insurance agencies and management agencies:
Fundamentally change the appraisal method, improve the efficiency and effectiveness of health insurance appraisal, and shorten the appraisal time of health insurance treatment costs.
Immediately detect illegal payment requests, promptly coordinate with medical facilities to inspect, adjust, and improve the effectiveness of controlling the use of health insurance funds.
Timely detect and prevent the situation of profiteering and abuse of health insurance fund. The results of automatic and proactive appraisal in 2017 showed that 100% of electronic records were controlled regarding information of health insurance participants, benefit levels, entitlements and established rules on conditions and payment levels for drugs, technical services and medical supplies.
There is a nationwide centralized database with specific information to serve the management and operation of the Health Insurance Fund and timely assessment, recommendation for adjustment, and development of Health Insurance policies.
Lessons learned
With the above achievements, Vietnam Social Security has successfully implemented, earlier than the requirement "Before 2018, complete the connection of IT software system between Social Security agencies and medical examination and treatment facilities to improve administrative procedures in medical examination and treatment, enhance the efficiency of health insurance appraisal, management and use of health insurance funds" assigned by the National Assembly in Clause 4, Article 2 of Resolution No. 68/2013/QH13 dated November 29, 2013 of the National Assembly and Resolution No. 36a/NQ-CP dated October 14, 2015 of the Government on e-Government.

Improve digital transformation in health insurance appraisal activities.
To effectively implement the Government 's direction in Resolution No. 50/NQ-CP dated April 17, 2020 and the programs and plans for digital transformation implementation of Vietnam Social Security, units assigned to carry out digital transformation need to proactively develop specific action programs, set out tasks and key solutions for implementation such as:
- Advise the Industry leaders to complete regulations, processes, and instructions on expertise and profession in the direction of IT application;
- Accelerate the digitization, updating and standardization of all relevant data databases;
- Prioritize key tasks in the digital transformation process;
- Coordinate well with specialized units to ensure IT infrastructure, security and information safety during implementation;
- Training, fostering expertise and qualifications, discovering talented cores to serve digital transformation;
- Stimulate innovation, creativity and application of science and technology of each civil servant.
Source


![[Photo] The 1st Congress of Phu Tho Provincial Party Committee, term 2025-2030](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/9/30/1507da06216649bba8a1ce6251816820)

![[Photo] General Secretary To Lam, Secretary of the Central Military Commission attends the 12th Party Congress of the Army](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/9/30/9b63aaa37ddb472ead84e3870a8ae825)
![[Photo] Solemn opening of the 12th Military Party Congress for the 2025-2030 term](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/9/30/2cd383b3130d41a1a4b5ace0d5eb989d)
![[Photo] General Secretary To Lam receives US Ambassador to Vietnam Marc Knapper](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/9/29/c8fd0761aa184da7814aee57d87c49b3)




























![[Photo] General Secretary To Lam attends the ceremony to celebrate the 80th anniversary of the post and telecommunications sector and the 66th anniversary of the science and technology sector.](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/9/29/8e86b39b8fe44121a2b14a031f4cef46)





























































Comment (0)